Table of Contents
Bariatric Surgery in Turkey: How to Find the Best Clinics?
Understanding Obesity Disease
You have decided to apply for bariatric surgery as a solution to get rid of your obesity problem, which you have been struggling with for a long time and which disrupts your health, psychology and comfort of life. We congratulate you on your decision and would like to explain once again how correct it is to take this step with some scientific facts.
Despite the 16 years we have spent to introduce and popularise this type of surgery in our country, it is still seen by many people as an “easy way out” to resort to surgery to get rid of excess weight. First of all, you should know and explain to the people closest to you that the obesity problem that has passed a certain stage is not a problem that can be solved by one’s own will, it is a much more complicated and severe health problem. Obesity surgery is not the “last” but the “only” and “best” remedy for this health problem, which has been registered as a “disease” by the World Health Organisation since the 1990s.
Then, let’s first explain the concept of obesity a little bit. Obesity, in the shortest definition, is an abnormal increase in the proportion of body fat. A person is considered obese if his/her body weight is 20 per cent above what it should be. The most practical measurement used in the evaluation of obesity is the body mass index (BMI) value calculated by dividing the weight by the square metre of height. It is accepted that the most important causes of obesity are excessive and wrong nutrition and lack of physical activity.

Which Health Risks Does Obesity Cause?
Health problems caused by obesity are as follows:
- Cardiovascular Problems: Coronary heart disease, congestive heart failure, occlusive vascular disease, venous stasis in the legs, varicose veins
- Type 2 diabetes
- Some types of cancer (uterine, breast, prostate and colon)
- Hypertension
- Dyslipidaemia (increased cholesterol and triglyceride levels in the blood)
- Stroke
- Digestive system problems: Fatty liver, gallstones, gastroesophageal reflux disease
- Respiratory tract problems: Sleep apnoea, hyperventilation syndrome, pulmonary embolism
- Musculoskeletal problems: Osteoarthritis (deterioration of articular cartilage), immobility, herniated disc
- Urogenital problems: Menstrual irregularities or missed periods, polycystic ovary, infertility, urinary incontinence.
- Psychosocial problems: Incapacity for work, social discrimination, depression
Obesity is a major health problem as it is the main cause of many diseases and impairs general health. For example, cardiovascular diseases, especially heart attack and stroke, are the number one cause of preventable deaths with 17 million deaths per year worldwide. The most important preventable causes of cardiovascular diseases are smoking and obesity. In addition, deaths due to Type 2 diabetes, which is directly related to obesity, will increase by 50 per cent in the next decade.
If the mortality rate is taken as 1 when the BMI is between 20-25, there is no significant increase between 25-30, but this rate increases 1.5 times after 30, 2 times between 35-40 and 2.5 times after 40. The risk of comorbidities such as diabetes and hypertension increases significantly after BMI 30.
Obesity is a multifactorial disease in which many causes play a role together. Among these, excessive and wrong nutrition and lack of physical activity are recognised as the most important causes. Therefore, it is not just about you “holding your throat” as the people around you may claim. First of all, you should understand and explain this. In addition, many genetic, environmental, neurological, sociocultural and psychological factors also play a role. The increasing rates of childhood obesity all over the world suggest that environmental factors are more prominent than genetic factors.
There are 4 main treatment methods (other than surgery) for obesity as summarised below. These are:
- Diet therapy
- Exercise therapy
- Medication
- Behaviour change therapy
It has also been proven by studies that once the body mass index exceeds 35, the chance of losing excess weight and maintaining it in the long term with methods other than surgery is between 0-5%, i.e. almost non-existent.

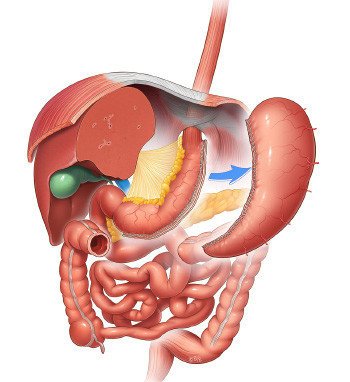
Understanding Weightloss Surgery
Obesity surgery or bariatric surgery is a term that includes a group of surgical methods applied on the digestive system in order to solve the problem of excessive weight that causes health problems and cannot be solved by methods such as diet and exercise. Although obesity surgery methods include many different surgeries, basically the mechanisms of action can be analysed in two groups. These are restricting the amount of food that can be taken (restrictive) effect and reducing the absorption of food (malabsorptive) effect.
A concept that you may come across frequently in articles on this subject is minimally invasive surgery, or laparoscopic surgery. This term refers to operations that can be performed with small incisions and special instruments without the need for a large incision in the abdomen.
In a minimally invasive type of surgery called laparoscopic surgery, or closed surgery, a total of 4 or 5 small incisions are made in the abdomen. These are usually no larger in diameter than your finger. Through special ports called trocars inserted through these incisions, laparoscopic instruments can access the abdomen. Meanwhile, carbon dioxide gas is filled into the abdomen at a certain pressure in order to prevent any injury to the intra-abdominal organs and to work comfortably. Most of this gas is discharged through the ports at the end of the operation, the remainder is absorbed by the peritoneum and excreted through the lungs. A side effect of this gas is that right or sometimes left shoulder pain is almost always experienced after laparoscopic surgery. This is a completely temporary side effect.
Laparoscopic surgery has many advantages over open surgery:
- Smaller, more aesthetic scars
- Less pain
- Shorter hospitalisation period
- Faster return to normal life
- Fewer wound site complications
The main purpose of obesity surgeries is to reduce the stomach capacity and the patient’s appetite on the one hand, as well as to provide healthy and permanent weight loss by breaking insulin resistance through a number of hormonal mechanisms. These surgical applications are a powerful tool you can use to help you lose weight, but no bariatric surgery method can guarantee permanent weight loss 100%.
Surgery is a key to regulating your eating and lifestyle. In order to achieve a permanent weight loss after surgery, you should follow the nutritional rules and increase your daily movement amount. Most importantly, you must be psychologically determined to permanently change the way you look at nutrition and your behaviour. Such an approach both increases the success of weight loss and prevents weight gain again. Diet after obesity surgery may vary according to the tolerance level of the person. Accordingly, it is possible to add or remove some foods.
The main procedures and operations performed within the scope of obesity surgery are as follows:
- Gastric Balloon (intragastric balloon)
- Sleeve Gastrectomy (sleeve gastrectomy)
- Gastric Bypass (Roux-en-Y or Mini Gastric Bypass)
- Revision Surgeries
- Duodenal Switch (SADI-S)
- Apollo Endoscopic Stomach Reduction
Gastric Balloon
Endoscopic intragastric balloon or gastric balloon is a non-surgical obesity treatment method. The gastric balloon, which was developed to fill the gap between diet and exercise alone and more complicated obesity surgery methods, has been widely used in recent years in overweight and obese patients who are not on the borderline of surgery.
There are many types of gastric balloon, but basically the mechanism of action in all of them is the same. The aim is to take up space in the stomach, reduce the feeling of hunger, and support the feeling of satiety with less food. With a diet and psychological support programme to be applied together, weight loss between 15-25 kg can be targeted in 6 months.
This method, which has almost no side effects other than stomach cramps, nausea and vomiting that can be seen in the first days after the procedure, is applied under short-term anaesthesia. After 6 months, the balloon is removed endoscopically in the same way.
Sleeve Gastrectomy
Gastric sleeve gastrectomy is technically the removal of the large part of the stomach (approximately 80%) that serves as a storage. Thus, the stomach, which normally has a volume of 1.5-2 litres, is converted into a thin tube with a volume of roughly 30-150 ml (roughly a large banana). As with gastric sleeve surgery, there is no foreign body inserted into the abdomen.
The aim is to reduce the amount of food that can be eaten at one time, but the natural flow of the digestive system is not interfered with in a way that reduces absorption. Since part of the stomach is removed, it is an irreversible surgery.
However, contrary to popular belief, sleeve gastrectomy is not only a volume restriction, but also a metabolic surgery. The removed stomach part secretes 90% of Ghrelin (hunger or appetite hormone) in the body. Removal of this part provides a significant control over appetite, especially in the first year.
Moreover, since Ghrelin is a hormone that works as the opposite of insulin, insulin resistance is broken after sleeve gastrectomy surgery, your body becomes able to spend the calories you take. In addition to these, the secretion of weight loss hormones secreted from the intestines increases due to some factors such as accelerated gastric emptying.
Gastric Bypass Surgery
Gastric bypass procedures are a group of similar operations used to treat morbid obesity, which is the excessive accumulation of excess weight in the form of fatty tissue in the body, leading to serious health problems.
In gastric bypass, the stomach is first divided into a small upper section and a larger lower section, called the “remnant”. The connections of both pouches to the small intestine are then reorganised. Compared to sleeve gastrectomy, these operations are more metabolically effective, faster and more weight loss. Since some of the excess calories are excreted while some of the vitamins and minerals are also excreted, vitamin and mineral levels should be monitored after the operation and supplements should be used when necessary.
Dumping Syndrome is a protective side effect of these surgeries in patients with a sweet diet. When refined sugars come into contact with the advanced parts of the intestines, symptoms such as sweating, palpitations and nausea develop. Thus, the patient realises that he/she is consuming a food that he/she should not consume and gradually moves away from these garbage foods.
Revisional Surgeries
Revision surgeries are secondary surgeries performed on patients who have previously undergone any obesity surgery, but either could not lose the desired weight or experienced weight regain, or experienced problems related to the surgery. In a sense, we can also call them corrective or transformative surgeries.
In revisional surgeries, whether the first surgery was performed in accordance with the technique affects the choice of surgery. For example, if the first surgery was a sleeve gastrectomy that was not performed in accordance with the technique, a sleeve gastrectomy can be performed again. However, if the first surgery was performed in accordance with the standards, it should be preferred to convert it into an absorption-reducing surgery.
The main difficulty in revision surgeries is the change in anatomy and adhesions in the abdomen due to the first surgery-operations. These factors may cease to be a risk only with the experience of the surgeon. It should be kept in mind that revision operations are higher level operations and should not be attempted except in experienced centres.
Duodenal Switch (SADI-S)
Duodenal switch surgery, also known as duodenal switch with biliopancreatic diversion, has been performed for a very long time. SADI-S is a more recent and safer modification of this highly effective operation.
Like gastric bypass, SADI-S has both restrictive and absorption-reducing effects. This method, which is also called loop duodenal switch surgery, is a highly effective surgery both in weight loss and in the solution of metabolic problems, especially diabetes, with both restrictive and serious absorption-reducing effects. In uncontrolled diabetic patients who use insulin, it has the power to stop the use of insulin as soon as it is performed.
Apollo Endoscopic Gastroplasty (Endoscopic Stomach Reduction)
Apollo endoscopic gastroplasty or endosleeve is a promising technique for the treatment of mild to moderate obesity. The long-term effects of the method have been proven by a large multicentre study. Between January 2013 and December 2015, patients who underwent the procedure in five centres were retrospectively examined. All methods were performed using the Apollo OverStitch device. Apollo gastroplasty method was performed for the first time in Turkey by our founder and lead bariatric surgeon, Dr Murat Ustun in 2014.

